ADRC First pre-screening project expanding statewide Jan. 3
New process means savings, quicker access to services
The ‘ADRC First’ pre-screening project has been extended and expanded, after a first phase saved the state an estimated $3.1 million.
Typically when Alaskans with age- or disability-related challenges came to care coordinators and other providers for support services, providers would apply to SDS on their behalf. To test a different process, the ADRC First pilot had providers in seven Central Kenai communities send new clients to their local ADRC (Aging and Disability Resource Center for pre-application screening instead.
Early this year, SDS staff analyzed data in the test area from Dec. 1, 2013 to Sept. 30, 2015 and found a 74 percent decrease in ALI (Alaskans Living Independently) applications and a 13 percent decrease in PCS (Personal Care Services) applications. During the same time period in the rest of the state, applications for both programs rose. Individuals in the pilot area got information and appropriate services with a quicker turnaround, because fewer people waited for assessments when they could be well served with community programs instead.
SDS researchers estimate 270 individuals were diverted from Medicaid programs, saving the state millions as well as connecting Alaskans to services faster.
Starting Jan. 3, 2017 the pre-application screening will be required for all individuals seeking long term care services and supports through the (ALI) and (APDD) Alaskans with Physical and Developmental Disabilities) Medicaid waivers. They will get a pre-screen and options counseling in person, over the phone, or by video prior to selecting a care coordinator and submitting an application for services.
The Alaska Mental Health Trust is contributing $400,000 to fund the expansion. Contacts: Martin Morris, 465-4798, martin.morris@alaska.gov; Lisa Morley, 465-4996, lisa.morley@alaska.gov.
![]()
Growing community, making connections
Juneau artist Luis Hernandez leads a class at The Canvas, an art studio that offers both day habilitation classes for Alaskans with disabilities, such as Hernandez, and community art classes. Part of the studio’s mission is helping clients develop as artists, including by teaching classes. Hernandez is instructing a printmaking class |
Thank you, Alaska providers, for turning in your self-assessments on compliance with the CMS rule that service settings must include participants in their local community.
Because of the large volume of assessments and limited staff, the evaluation period will take months.
"This is a heavy lift for us,” said SDS Director Duane Mayes.
If an agency’s self-assessment and stakeholder feedback point to the need for change, SDS technical assistance consultants are here to help, said Program Manager Jetta Whittaker.
“We’ll also be validating the assessment results with participants,” said Whittaker. “It’s not necessarily a geographic thing. It’s about how welcoming your agency is. Is it open to the community?”
Questions? Contact Whittaker at 465-1605.
![]()
January care coordinator conference, new training, and thanks!
SDS is holding a care coordinator conference Jan. 18-19 in Anchorage at the Sheraton hotel. The topic line up will feature keynote speakers SDS Director Duane Mayes and Ric Nelson of the Governor’s Council on Disabilities and Special Education; an orientation on the division’s new electronic case record system; a first-time-ever class for people who would like to become care coordinators, and a “Provider Showcase.”
High-interest sessions include guardianship and advocacy; helping people with complex behavioral needs, and Dr. Adam Grove with the Alaska Brain Injury Network will present “Holistic approaches to identifying and treating traumatic brain injury”.
High-interest sessions include guardianship and advocacy; helping people with complex behavioral needs, and brain injury facts and insights from Dr. Adam Grove with the Alaska Brain Injury Network.
“We have a lot of cool topics,” said Kara Thrasher-Livingston, SDS training program manager.
The electronic record system, for example. Known as Harmony and Mediware, the system has been underway for years, pulling together several separate and outdated (even paper) record systems. Now, the vision of an electronic file that different personnel can access — applicants, care coordinators, SDS staffers, etc. — is close to becoming a functional reality. The records will be secure, with each personnel type only able to access the information relevant for their role.
“We’ll have a session that tells care coordinators how to get ready for it,” Thrasher-Livingston said.
There will also be a new training, “Basic Concepts of Care Coordination” presented in partnership with the Center for Human Development, housed at the University of Alaska Anchorage. It gives people who have never been care coordinators an overview of what’s entailed.
The Provider Showcase fair wasn’t possible before, but now that conflict-free rules are in place, providers and agencies like the Governor’s Council will have booths explaining what they offer.
Care coordinators can register for the conference at https://www.eventbrite.com/e/care-coordinator-connections-2017-tickets-28346817093.
Many thanks
Many thanks, care coordinators, for submitting your conflict-free attestation and assurance forms.
The division encourages any providers who applied for exceptions to the conflict-free rules to think about ways to move beyond the need for an exemption.
“The goal is to have all areas of the state be conflict-free in the future,” said SDS Deputy Director Deb Etheridge.
Forms and information are on the SDS CFCC webpage.
![]()
Update on 1915 (i) and (k) options
After careful consideration, SDS is looking more closely at a 1915(i) option for Alaskans with Alzheimer ’s disease or related dementia.
The contractor evaluating whether 1915 (i) and (k) options were workable in Alaska supported the (k) option but recommended against the four (i) options under review.
The contractor’s feasibility study, released at the end of July, identified alternative paths for serving the other three (i) target populations: Alaskans who experience intellectual and developmental disabilities, those who experience traumatic brain injury, and those who experience serious mental illness. The study said there were no other clear alternatives for Alaskans with dementia, however. For that reason, we’re taking a second look at the (i) option, and have developed a new concept paper. We’ll keep you posted. The Community Council, the state’s advisory group on 1915(i) and (k) possibilities, has met monthly since Oct. 2015.
The Council is comprised of elderly Alaskans, Alaskans with disabilities, and their representatives. The council’s page on SDS’ website links to meeting notes.
Good to have you aboard, State Independent Living Councils and Infant Learning Program!
The SILCs became part of SDS in July. They were previously housed in the state Department of Labor and Workforce Development.
The Infant Learning Program moved into SDS’ building on Eighth Avenue in Anchorage this past summer, after being housed in the Office of Children’s Services for some time. Maureen Harwood, manager of the Intellectual and Developmental Disabilities unit, now oversees the program.
We’re excited to have been able to welcome these programs – they’re a great fit with the SDS mission and suite of programs.
![]()
DD Registry shrinks, thanks to dedicated
SDS staffers
A huge “Well done!” and “Thank you!” to Katie Schoenwetter and Jeremy Meade for setting themselves the mission of making the developmental disability registry more accurate and up-to-date, connecting many waiting Alaskans with services in the process.

Schoenwetter said they really went after the list starting in July of 2015, and have brought the number of names down to 545 from close to 800.
“Jeremy and I are doing our best to steadily reduce the number of people on the registry,” Schoenwetter said. “We’ve made it more of a routine to keep going through it, to make it more accurate.”
The pair has worked hard to identify people who no longer need services and can be removed from the registry, because they’ve moved out of state or for some other reason. Then Schoenwetter and Meade work to connect individuals who are still interested with nearby short-term assistance and referral (STAR) professionals who can help them fill out the developmental disability determination forms that start the application process. The STAR folks can also help them apply for grant services while they’re waiting.
“It was a lot of work,” Schoenwetter said, but very worthwhile. “It’s a little surreal. After all the letters we sent out, after being in such a long process, it was nice to start seeing progress.”
Caitlin Rogers, the team’s supervisor, said they go above and beyond their role as support staff for the unit.
“To have people who really understand the importance of keeping that list current is really special,” Rogers said. During a time when state funding is reduced and the division is short-staffed, Rogers said the tremendous effort the two have put into serving Alaskans is deeply heartening for the whole division.
Schoenwetter said the progress was heartening to her and Meade as well: “It feels great.”
![]()
Telehealth advances
SDS has finished its telehealth policy, posted here, and is exploring the possibility of remotely assessing people in their own home.
SDS is piloting a new platform that would allow an assessor to videoteleconference with recipients in their homes through a secure connection.
This platform is also being tested by state care coordinators to meet with clients who are in out-of-state treatment facilities.
SDS began experimenting with telehealth a few years ago, first doing re-assessments by videoteleconference. With budgets shrinking and demand rising, the division hired Tarik Thomas in January 2016 to expand the division’s telehealth services.

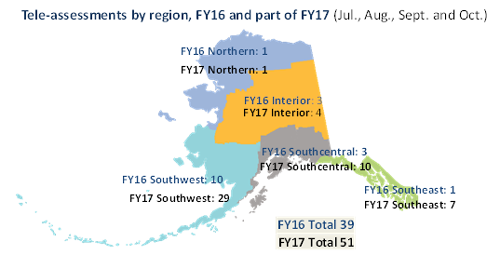
At that time, three rural health care agencies had signed up to offer assessments for Medicaid and Personal Care Assistance (PCA) recipients via telehealth. Now a dozen providers all around Alaska have signed up, and are using videoteleconferencing for initial as well as re-assessments.
Expanding telehealth is shrinking assessment costs.
The division saved an estimated $45,800 in FY16; after only four months in FY17, the division has seen more than $44,000 in estimated savings from more than 50 tele-assessments.
Local providers go through paperwork with applicants before the assessment. Then from a private room in Anchorage, an assessor videoteleconferences with the provider and applicant or client. The video link allows the assessor to speak with the individual and observe his or her movements.
The paperwork that care coordinators need to help applicants prepare before the assessments are on the SDS forms page under Telehealth.
Thomas developed a brochure on the process for agencies to share with applicants. There is also an environmental questionnaire to help assessors understand recipients’ and applicants’ living conditions. These are on the telehealth page on the SDS website.
The new policy on using telehealth for assessments is posted on the SDS policy page. It outlines the documents that recipients and applicants must submit before their assessment, as well as the steps SDS completes. Our review of the reimbursement policy for facilitating remote assessments is still underway.


