Mpox (Monkeypox)
Mpox was formerly known as monkeypox
The Alaska Department of Health is closely monitoring mpox transmission to ensure rapid identification of cases and working with providers to offer vaccine to people who have been exposed to mpox or are most at risk for exposure.
While mpox can infect anyone, in the United States, clade II mpox is still mostly being spread through sexual and intimate contact, and gay, bisexual, and other men who have sex with men are at the highest risk of getting mpox. The risk of mpox to the general public is currently low.
Mpox is a rare disease that is caused by infection with mpox virus. Mpox virus belongs to the Orthopoxvirus genus in the family Poxviridae. The Orthopoxvirus genus also includes variola virus (which causes smallpox, which has been eradicated), vaccinia virus (used in the smallpox vaccine), cowpox virus, and borealpox virus. There are two types of mpox virus: clade I and clade II. Currently, only clade II mpox has been detected in the United States. An ongoing outbreak of clade I mpox is affecting the Democratic Republic of the Congo (DRC), with cases recently spreading to several neighboring African countries. On August 14, 2024, the WHO declared the DRC mpox outbreak a public health emergency of international concern. However, the risk of clade I mpox to the U.S. public remains low at this time, and there are no reported cases of clade I mpox in Alaska or elsewhere in the United States.
Mpox Surveillance In Alaska
What Alaskans Can Do
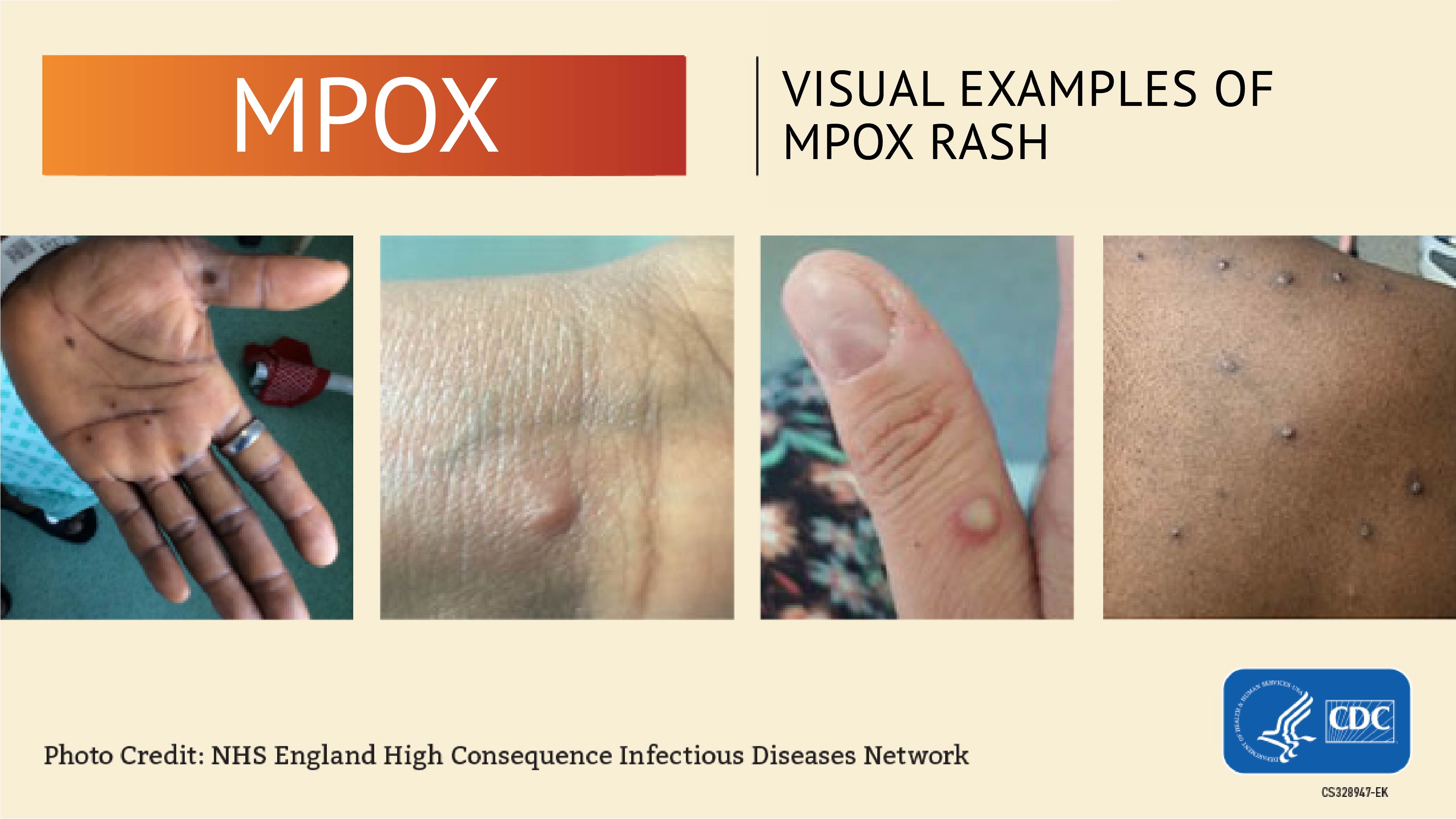
- People who are concerned that they may have mpox or anyone with a rash that looks like mpox (pimples, blisters or sores) should talk to their health care provider. If you do not have a health care provider, contact your
local public health center.
- Be aware that mpox can spread to others from the time symptoms start (before the rash forms) until all sores have healed and a fresh layer of skin has formed. This can take several weeks. There is evidence that some people can spread the virus 1 to 4 days before they develop symptoms, but it’s not clear how often this happens. Learn more about
How It Spreads on the CDC website.
- If you have symptoms of mpox isolate from others and contact a health care provider right away.
- Before visiting a health care provider, patients who are concerned they might have mpox should call ahead to let their health care provider know.
- Avoid close contact, including sex, with people who have mpox symptoms like sores or rashes.
- Do not handle or share the bedding, towels, or clothing used by a person with mpox.
- Always talk to your sexual partner(s) about any recent illnesses. Be aware of new or unexplained sores or rashes on your body or your partner’s body.
What Do I Do If I Think I Might Have Been Exposed?
Call your local public health center or health care provider right away and let them know you think you were exposed to mpox. Based on your situation, you might benefit from being given the JYNNEOS vaccine, which can help prevent infection if given early after an exposure.
Symptoms
Symptoms of mpox can include:
- Rashes, bumps, or blisters on or around the genitals or in other areas like your hands, feet, chest, or face.
- Flu-like symptoms, such as fever, headache, muscle aches, chills, and fatigue. These symptoms may occur before or after the rash appears, or not at all.
Symptoms develop approximately 7-14 days after a person has been exposed but may be as early as 5 days and as late as 21 days. The rash begins as a flat rash, then progresses to raised bumps which become filled with fluid. Eventually the rash crusts over and scabs develop. Some people may have only one sore, bump, or blister. This may look different from pictures you see online.
How It Spreads
Most infections occur from close, personal skin-to-skin contact with someone who has a mpox rash. Transmission is possible through:
- Prolonged direct contact with an mpox rash, scabs or body fluids from a person with mpox. This can happen during activities like kissing, hugging, massaging, cuddling and having sex.
- Touching objects or fabrics (bedding, clothing or towels) or sharing items such as toothbrushes, cups or utensils that have been used by someone with mpox.
- Contact with respiratory secretions during prolonged face-to-face contact.
Vaccines
The JYNNEOS vaccine can help prevent mpox and is recommended for people at high risk for mpox infection.
The vaccine can be administered:
- After exposure for people who have been exposed to mpox to reduce the risk of infection and serious illness OR
- Prior to exposure for people at high risk of exposure to prevent mpox infection
For vaccination after an exposure has occurred (but before symptoms have occurred), the vaccine is most effective when given within 4 days of exposure but can be given up to 14 days later. People who are severely immunocompromised may be considered for vaccine later than 14 days after exposure. If mpox lesions have already appeared on the skin, JYNNEOS vaccine is not recommended.
Who is recommended for vaccination?
Mpox vaccination is not recommended for the general public, but it is recommended for those at increased risk for infection. Transmission of mpox primarily occurs from close, personal skin-to-skin contact with someone who has an mpox rash.
-
Vaccination is available in Alaska for people who self-identify as being at increased risk for infection.
Mpox vaccination should be offered to:
- People who had known or suspected exposure to someone with mpox
- People who had a sex partner in the past 2 weeks who was diagnosed with mpox
- Gay, bisexual, and other men who have sex with men, and transgender or nonbinary people (including adolescents who fall into any of the these categories) who, in the past 6 months, have had:
- A new diagnosis of one or more sexually transmitted diseases (e.g., chlamydia, gonorrhea, syphilis); or
- More than one sex partner.
- People who have had any of the following in the past 6 months:
- Sex at a commercial sex venue; or,
- Sex in association with a large public event in a geographic area where mpox transmission is occurring.
- Sex in exchange for money or other items
- People who are sexual partners of people with the above risks.
- People who anticipate experiencing any of the above scenarios.
- People with HIV infection or other causes of immunosuppression who have had recent or anticipate potential mpox exposure.
- People who work in settings where they may be exposed to mpox:
- People who work with orthopoxviruses in a laboratory